Your heartbeat can tell a lot about you: your emotional state, how physically active you're being at any given moment, and even how much coffee you've had this morning. But it can also tell your physician how healthy your heart is.
When your physician listens to your heartbeat, he or she is hoping to hear a "lub-dub" sound. This means that the heart is beating properly -- the electrical signals that keep your heart beating are traveling through your heart in a regular pattern to get blood out of your heart and to the rest of your body.
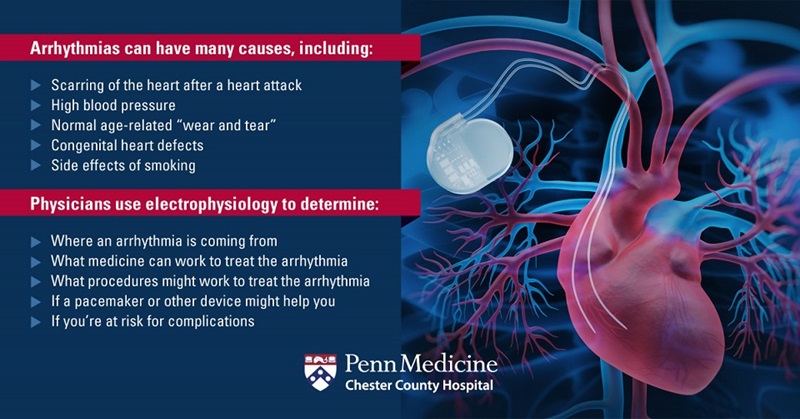
But if your heart is not doing that correctly, physicians can use a branch of cardiology focused specifically on the heart's rhythm -- called electrophysiology -- to figure out why.
Kurt Schillinger, MD, PhD, Chief of the Arrhythmia Program at Chester County Hospital, explains what electrophysiology is and how it can help regulate your heart's rhythm.
The Focus of Electrophysiology: Arrhythmias
Electrophysiologists study arrhythmias -- problems where your heartbeat is too fast, too slow, or irregular.
Sometimes, arrhythmias are completely harmless. But other times, they can be life-threatening.
If the arrhythmia is very short, it might not affect your heart rate enough to cause any harm. But if it lasts long enough, it can cause your heart to pump less effectively. As a result, your body doesn't get the blood it needs.
What Happens During an Electrophysiology Study?
An electrophysiology study (EPS) is a test that records your heart's electrical activity. It lets the electrophysiologist know if it's beating as it should or if you'll need treatment to get it back in rhythm.
 "Not everyone with an arrhythmia needs an electrophysiology study. Depending on your age, risk factors, and preferences, we may try to manage your arrhythmia with medicines. However, if you cannot tolerate medicine, or if medications are not successful, then an electrophysiology study can be considered," explains Dr. Schillinger.
"Not everyone with an arrhythmia needs an electrophysiology study. Depending on your age, risk factors, and preferences, we may try to manage your arrhythmia with medicines. However, if you cannot tolerate medicine, or if medications are not successful, then an electrophysiology study can be considered," explains Dr. Schillinger.
During an EPS, your physician will insert a small, straw-sized tube (sheath) into an artery in your groin, neck, or arm. Using this sheath, a special catheter (flexible tube) will be guided into your blood vessel to access your heart. Your physician will then send small electrical pulses to your heart to make it beat at different speeds, and he or she will record your heart's activity to determine where the arrhythmia is coming from.
While you might feel your heartbeat changing pace, it shouldn't be uncomfortable -- your physician will numb the area he or she is working on, as well as give you a sedative, so you can relax and not feel pain during the procedure. The whole procedure takes about 1 to 4 hours. It's an outpatient procedure, meaning you can go home the same day.
If your physician plans to use a treatment called ablation, he or she will use the EPS to put the heart into the specific arrhythmia being targeted. "This is an important step in the process, as it allows the electrophysiologist to confirm the cause of your arrhythmia, as well as the location of abnormal circuits in the heart that are causing it," Dr. Schillinger says.
How Your Arrhythmia Can Be Treated
If your physician is able to determine the type and location of the arrhythmia, there are treatments to help your heart beat regularly. This may be scheduled for a later date, or it may be done immediately after the electrophysiology study.
Ablation
Ablation is similar to an EPS study because it uses catheters to access the heart. However, ablation uses mild, painless, radiofrequency energy to destroy the tissue in the heart that's causing the arrhythmia. This allows your heart to get back to its regular rhythm.
Implantable Devices
Implantable devices attach to your heart to help it beat as it should. These devices include different types of pacemakers and defibrillators.
Pacemaker
A pacemaker is a small device with tiny wires that are connected to your heart. It produces electrical impulses to make your heart beat, timing it to beat at regular intervals. A pacemaker is usually implanted under your skin next to your heart, but it can also be external and temporary.
His-bundle Pacing
Pacemakers apply energy to one side of the heart, which Dr. Schillinger says can worsen the heart's functioning in some patients. At Chester County Hospital, His-bundle pacemakers are used to keep your heart functioning more efficiently.
"His-bundle pacing requires the implantation of a special type of cardiac pacemaker, which has the ability to apply energy directly to the heart's normal conduction system. By using the normal conduction system of the heart, these pacers are capable of ensuring that electricity from the pacemaker travels to both sides of the heart simultaneously," Dr. Schillinger says.
MICRA™
At Chester County Hospital, a new form of pacemaker technology called MICRA is available.
"Traditional pacemakers use a computer or 'pulse generator,' which is implanted under the skin on the upper left chest. This pulse generator is connected to the tissue of the heart by wires that travel from the computer down to the heart through veins from the arm," explains Dr. Schillinger.
With MICRA, however, the pulse generator and wires are integrated into a single piece that is shaped like a bullet. MICRA is placed entirely within the heart using an X-ray system and a special delivery tube that brings the device to the heart while you're sedated.
Dr. Schillinger adds, "One of the great things about MICRA is that the recovery time after implantation is significantly shorter and much easier. With a traditional pacemaker, you would have about 6 weeks of restricted arm motion. But with MICRA, there is no need for restrictions."
Implantable Cardioverter Defibrillator
An implantable cardioverter defibrillator (ICD) is a device that is used for the prevention of sudden cardiac death in patients who have a predisposition to dangerous arrhythmias.
This pager-sized device monitors your heart's rhythm and can deliver a shock if a dangerous arrhythmia is detected. This shock restores your heart to its normal rhythm, reducing the risk of suffering from a cardiac arrest.
ICDs are surgically placed into the chest and one or more flexible leads run from the device through your veins to the heart. ICDs may also be used as a pacemaker to regulate your heartbeat.
Subcutaneous ICD
A subcutaneous ICD (S-ICD) is a new type of ICD available at Chester County Hospital. Unlike traditional ICD implants, the device is placed entirely under the skin and does not require leads in the heart, leaving the vascular system untouched.
"S-ICDs significantly decrease the risk of infections in the bloodstream and heart valves since there are no components in the vascular system," Dr. Schillinger says. "And just as with MICRA, the S-ICD has fewer motion restrictions after implantation."
S-ICDs specifically provide defibrillation therapy for patients who do not have symptomatic bradycardia, which is when your heart beats slower than normal, or for patients who require pacing.
Chester County Hospital's Electrophysiology Lab
Chester County Hospital's electrophysiology lab uses state-of-the-art equipment, which gives clinicians the ability to provide the safest and most effective care for patients.
"The electroanatomic mapping system -- which physicians use to guide procedures like ablation -- is the most up-to-date system available in the United States," Dr. Schillinger says. "This system allows us to create a 3D representation of a patient's heart in real-time."
The lab also uses Jet Ventilation, a special type of mechanical ventilation in intubated patients -- patients using breathing tubes -- that reduces the movement of the heart during breathing, which ensures that the ablation is most effective.
The electrophysiology lab also uses Intracardiac Echocardiograph -- a special type of ultrasound imaging which allows providers to look at heart structures and catheters inside the heart in real time.
Dr. Kurt Schillinger, Chief of the Arrhythmia Program,
explains how Chester County Hospital's ablation lab in the invasive
cardiovascular suite compares to others in our area.
Prioritizing Your Heart Health
By keeping your heart's rhythm regular, you'll lower your risk of potentially life-threatening complications, like a heart attack.
Your primary care provider is your first step in monitoring your heart health. Your provider will listen to your heart and determine if you need further testing. From there, your care team can determine if you need an electrophysiology study and how you can get your heart's rhythm back to the "lub-dub" you know and love.
If you have questions about your heart health or electrophysiology services at Chester County Hospital, call 610-220-0432 to speak with a Heart and Vascular Nurse Navigator.
Approximately 2.7 million Americans suffer from Atrial Fibrillation, a form of arrhythmia, or irregular heartbeat. Download our guide on Atrial Fibrillation.
Related Information from Chester County Hospital: