
Joan, recovered breast cancer patient at Chester County Hospital.
Rattling as a breast cancer diagnosis is, treatments are more effective than ever before. That's partly because they're more personalized than they've ever been. This is a glimpse at what the journey -- from diagnosis to restoration -- looks like at Chester County Hospital.
A breast cancer diagnosis can arrive like a shock, simultaneously rocking both your equilibrium and plans for the future. Once that moment begins to subside, however, there are many reasons to be hopeful. In recent years, treatment options have grown in number and effectiveness, which has enabled doctors to better tailor their care to a patient's specific needs. As a result, breast cancer, when caught early, is nearly always cured.
As an integral member of the Penn Medicine healthcare system, Chester County Hospital has been able to aggressively combat breast cancer. High-caliber surgeons are deploying the full range of available tactics to not only achieve a successful outcome but also to completely restore patients’ quality of life for the many years that will follow their treatment.
Here, we'll describe what this journey looks like at The Abramson Cancer Center at Chester County Hospital, from diagnosis to breast reconstruction.
Tailoring the Treatment

Oncologic surgeon Susan S. Chang, MD, did her fellowship training at the John Wayne Cancer Institute. At the time, she was simply trying to become a more proficient surgeon. She had no expectation of building her career around breast health. But as she progressed through the final phase of her training, she grew to appreciate the deeper and more enduring relationships she was forming with her patients.
Joan appreciated Dr. Chang's thorough approach to her treatment. After a scare in April 2021 she followed an aggressive screening schedule, enabling her care team to catch a cancerous tumor very quickly.
"It's very different from when, say, someone gets an appendectomy, or they have their gall bladder taken out. Once they're done, they’re done. You don't see your surgeon again unless you have another surgical problem," Chang says. "But as a breast cancer surgeon, I'm doing surgical procedures and I'm remaining in my patients' lives through their entire treatment and, hopefully, for many years after that."
A patient typically will meet with Chang after they've been diagnosed by their family doctor or gynecologist. Because most women undergo a mammogram as a matter of routine, many of Chang's patients are diagnosed relatively early in the course of their disease, which enables her to discuss breast-conserving therapy (the cancer is removed while leaving as much of the breast intact as possible) as well as mastectomy.
But treatment is rarely an either-or scenario. It can include some combination of surgery, radiation therapy, chemotherapy, hormone therapy, HER2-targeted therapy, CDK4/6 inhibitor therapy, immunotherapy, or PARP inhibitor therapy.
"It's also not straightforward, where everyone goes down this one path," Chang says.
How much the cancer has spread will heavily influence the course of treatment. But the patient';s age and their family history with the disease are also taken into account. For that reason, Chang will often order additional imaging studies, including a breast MRI, as well as genetic testing.
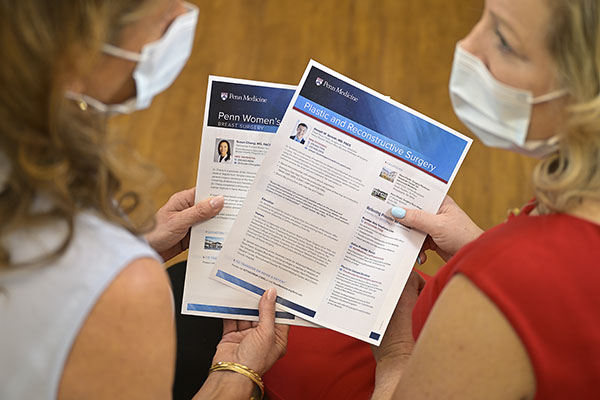
"When we meet, nothing's set in stone because I'm still gathering information that could totally change the surgical management," she says. "Still, it's pretty overwhelming. Usually we tell patients, bring a family member or friend, a second set of ears, because it's a lot of information thrown at them."
For reference later on, she provides her patients with a binder and book published by SHiNE – a donation-based support initiative the Chester County Hospital Foundation fosters for cancer patients in Chester County. She'll also advise them to limit their Googling and the number of people they confide in about their diagnosis. The reason is largely the same for both: there's a lot out there. In the end, very little of it will apply to you. So, spare yourself the stress of worrying about it.
She's commonly asked, "What would you do?"
She always declines to answer. "Everybody's different," she says. "I don’t want them to make their decision based on what I would do for myself in this situation."
While she is the surgeon, Chang wants to make sure each of her patients has agency over their treatment. She'll explain their diagnosis, the stage of their disease, and the options available for curing it. But she prefers, once all of the best clinical options have been presented to them, that the patients decide which course is right for them.
Surgery is generally scheduled a month after the initial meeting with Chang, though it can vary based on the timing of the imaging studies, whether the patient decides to undergo another kind of treatment prior to their operation, and if they opted for breast reconstruction following their treatment.
A new collaboration with the office of Joseph M. Serletti, MD, FACS, Chief of Plastic Surgery for Penn Medicine and the Henry Royster-William Maul Measey Professor in Plastic and Reconstructive Surgery at the Perelman School of Medicine at the University of Pennsylvania, offers patients the option to have an immediate reconstruction following their mastectomy. When patients are candidates for this option and interested in learning more, Chang will arrange for a consultation.
Drs. Chang and Serletti began working together at Chester County Hospital last fall.
"It's been wonderful working with him," Chang says. "He's bringing a lot of different options to our patients at Chester County Hospital. And the outcomes have been great."

"Dr. Chang treats you like you are the only patient she has when you are with her. Her bedside manner is wonderful and I trust her immensely."
Restoring What Was Lost
Though breast reconstruction surgery follows treatment, Serletti believes a woman should be informed about it the moment a mastectomy becomes a possibility. As much as it is a matter of awareness, it's also about ensuring the patient has sufficient time and space to decide. Everyone, he says, will come to the decision to do it, or not do it, in their own way because it’s weighted with a significant emotional component.
"Breasts are an important part of a woman's body and, in turn, her identity and perception of her sexuality,” he says. “Restoring them to their previous state can have an enormous psychological impact. Many studies have shown breast reconstruction can positively influence a woman’s wellbeing.”
There are two ways to reconstruct a breast. One is with an implant and the other makes use of the patient’s own tissue. The implant is the more traditional approach, though the tissue reconstruction tends to yield a more natural result, Serletti says.
He has performed both procedures at Chester County Hospital. "What we're doing at the Hospital of the University of Pennsylvania, we're also doing at Chester County Hospital," he says.
The implant reconstruction is a three-step process. First, Serletti will place an inflatable balloon under the skin of the breast and fill it partway so that the patient’s left with the beginning of a breast mound. Then, two weeks after the surgery, she'll begin a series of weekly in-office treatments during which Serletti will add a little saltwater to the balloon, slowly stretching the skin so that it will ultimately be able to accommodate an implant the size of the patient's original breast. Typically, this process occurs over about three months.
Finally, during a one-hour procedure, Serletti will remove the balloon and place the implant.
That said, working together, he and Chang have been able to expedite the process and move straight to placing the implant with a few patients. "They’ve gone incredibly well," he says. "The patient spends one night in the hospital."
When the patient's own tissue is used to reconstruct the breast, the tissue is usually taken from her lower abdomen. "It's basically like a tummy tuck, only instead of discarding the tissue, we're using it to reconstruct the breast," Serletti says. "It's a little more of a complex operation than the implant, but the entire breast is reconstructed in a single day."
For an implant reconstruction, a patient generally will spend a night in the hospital after the surgery and then another four weeks recovering at home. A tissue reconstruction entails a three-day hospitalization, followed by six weeks of recovery at home. At the six week-point, with both procedures, the patient is usually permitted to resume all normal activities.
Whether to undergo breast reconstruction is not an easy decision to make, especially after a lengthy treatment, but Serletti says he's rarely seen someone regret doing it. The opposite, in fact.
"Once she's fully recovered, she'll see the very natural-looking result and say she really underestimated how important this was to her," he says. "And that's very rewarding for me, to help someone reach that emotional state where they're feeling good about themselves again."
"You want what's best for you, and the best medical care after a breast cancer diagnosis," Rimkis added. "Dr. Serletti is the best. He is extremely calm and gentle. He provides answers to your questions and gives you all of the information about the options and procedure."

Cynthia Brown, BSN, RN, CN-BN -- Breast Care Coordinator.
Steering one's way through a cancer diagnoses is made easier for patients thanks to a the compassionate care they receive from our clinical teams, including Cynthia, one our nurse navigators. Learn More!
|